The Programme of Assessment
The programme of assessment lays out how pharmacists will be assessed against the curriculum outcomes and the tools available for formative and summative use.
- Individuals undertaking this programme will be required to compile an electronic portfolio evidencing their learning against the curriculum outcomes in line with the programmatic assessment principles defined above
- Using a variety of formative and summative assessment instruments evidencing their learning, referring to the descriptors to help guide them on the level of performance required, individuals will be able to demonstrate their achievement of the learning outcomes
- The RPS has sought to provide sufficient guidance as to when and how to use each assessment instrument whilst allowing the individual and their expert mentors and professional coach the freedom to make an informed judgement as to which method or combination of methods are most appropriate in any given learning situation
- For some higher-stakes outcomes, mandated assessment guidance has been stated; this means that evidence mapped to these outcomes must include examples of these assessment types to be achieved
- Collaborators, including expert mentors and professional coach, will be given access to the RPS e-portfolio to undertake supervised learning events, record feedback and provide judgements and narrative against the learning outcomes
- Individuals will also be able to record the outcomes of their meetings with their expert mentors and professional coach using the relevant report templates and develop action plans to inform next steps
Supervised Learning Events (SLEs)
A range of assessment instruments are included within the RPS consultant pharmacist e-portfolio that individuals undertaking the programme, as well as their collaborators, can use to record learning and demonstrate progress towards the curriculum outcomes.
The tools below can be used to demonstrate learning; however, individuals may choose to upload other forms of evidence to their portfolio to demonstrate their learning.
|
Work-based assessment instrument
|
Purpose
|
|
Directly observed procedure (DOPS)
|
To evaluate the performance of an individual in undertaking a clinical procedure.
|
|
Mini clinical evaluation exercise (Mini-CEX)
|
To evaluate a global clinical encounter with a patient assessing the synthesis of skills essential for clinical care such as history taking, communication, examination and clinical reasoning.
|
|
Direct observation of non-clinical skills (DONCS)
|
To evaluate the pharmacist’s non-clinical skills.
|
|
Acute care assessment tool (ACAT)
|
To evaluate the pharmacist’s clinical assessment and management, decision making, team working, time management, record keeping, prioritisation and handover over a continuous period of time across multiple patients.
|
|
Case-based discussions (CbDs)
|
To retrospectively evaluate the pharmacist’s input into patient care. A structured discussion is undertaken remotely from the patient(s) and is used to explore the clinical reasoning, decision making and application of complex clinical knowledge in practice.
|
|
Case presentation (CP)
|
To evaluate the pharmacist’s ability to effectively present a case to colleagues demonstrating effective clinical assessment and management, decision making, team working and time management.
|
|
Journal club presentation (JCP)
|
To evaluate the pharmacist’s ability to effectively present a journal paper to colleagues demonstrating knowledge of research methods and critical evaluation skills
|
|
Patient survey (PS)
|
To evaluate the pharmacist’s communication and consultation skills from the patient’s perspective.
|
|
Patient survey summary reflection (PSR)
|
To evaluate the pharmacist’s ability to reflect on and identify areas of development based on patient feedback.
|
|
Teaching observation tool (TO)
|
To evaluate the pharmacist’s ability to deliver an effective learning experience to others.
|
|
Reflective accounts (RA)
|
To evaluate the pharmacist’s ability to reflect on an experience, analyse their learning and identify areas of development to inform future practice.
|
|
Quality improvement project assessment tool (QIPAT)
|
To evaluate the pharmacist’s ability to undertake a quality improvement project to improve service provision in their area of expertise.
|
|
Multiple source feedback tool (MSF)
|
To evaluate the pharmacist’s level of performance in the relevant domain.
|
|
Leadership assessment skills (LEADER)
|
To evaluate the pharmacist’s non-clinical leadership and team working capabilities
|
|
Expert mentor report (EMR)
|
To evaluate the pharmacist’s overall performance and progress in the relevant domain/s.
|
|
Professional coach report (PCR)
|
To evaluate the pharmacist’s overall performance and progress towards achieving the consultant pharmacist outcomes.
|
Evidence types additional to supervised learning events will also be required to demonstrate achievement of the curriculum outcomes. The individual undertaking this programme is free to upload any evidence type they feel demonstrates achievement of the curriculum outcomes.
Examples could include, but are not limited to, the following:
- Published journal articles
- Evidence of published research
- Copies of anonymised written feedback from patients and stakeholders
- Copies of anonymised documents evidencing active involvement in the design of care pathways
- Videos or recordings of presentations and/or meetings.
Assessment blueprint and evidence requirements
The blueprint below shows the recommended assessment instruments for each outcome; it is, however, at the individual’s discretion as to which assessment instruments they choose to evidence each outcome. It is not expected for the individual to use all the recommended potential instruments – these are provided simply as guidance and the assessment tools used will depend on the nature of the learning and the educational context.
The level of stakes for each outcome was determined by the consultant pharmacist task and finish group and is based on each outcome’s potential risk to patient harm. All the curriculum outcomes should be considered as equally important in terms of demonstrating consultant-level practice and all outcomes must be achieved in the programme of assessment to pass.
ACCESS THE ASSESSMENT BLUEPRINT
Back to the top
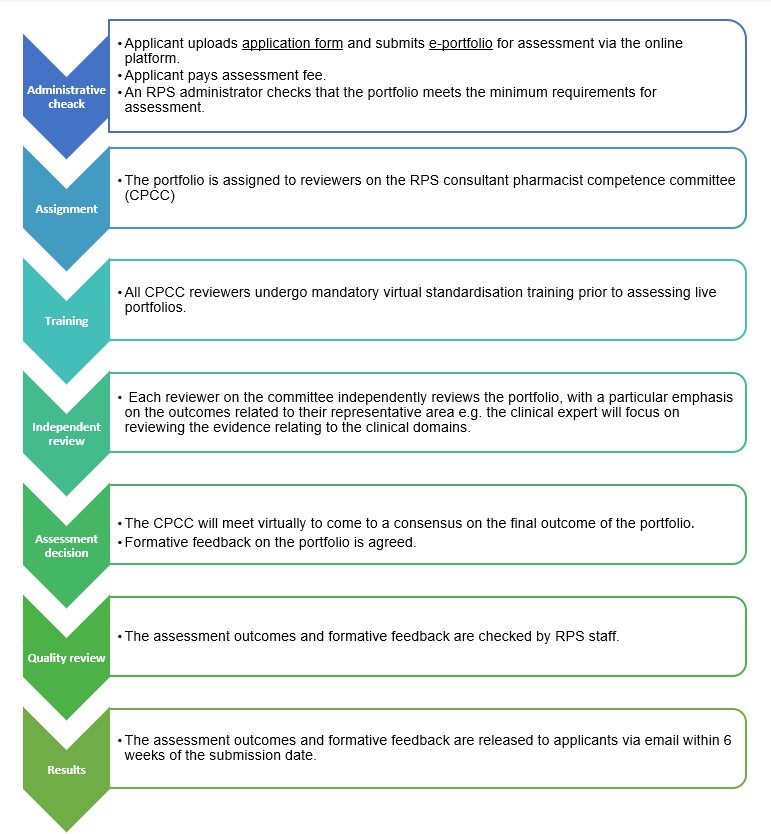
The assessment process
Throughout the credentialing process, you will need to maintain an e-portfolio of your learning and evidence using the RPS consultant pharmacist e-portfolio. The assessment process is shown below: