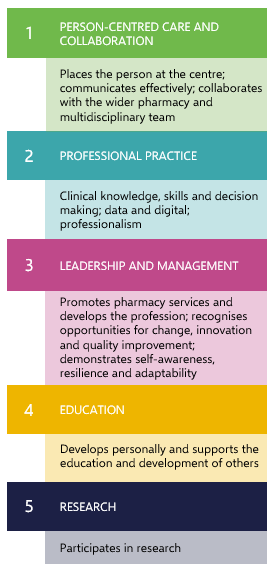
The post-registration foundation pharmacist curriculum is made up of five domains, each comprised a set of capabilities, outcomes and descriptors.
Key definitions
Domains
Collections of commonly themed capabilities and outcomes. There are five domains in the post-registration foundation pharmacist programme of learning.
Capabilities
High-level, complex professional capabilities are flexible and adaptive in a wide range of contexts and synthesise the knowledge, skills, behaviours and experience pharmacists need to manage real-life scenarios. Each of the domains in this programme of learning is made up of between one to four capabilities and there are 13 capabilities in total.
Outcomes
Describe what is to be achieved by pharmacists by the end of the programme; these describe the knowledge, skills, behaviours and experience of those who successfully complete the programme of assessment.
Descriptors
Detail the level and breadth of performance required to satisfactorily meet the curriculum outcomes. They provide greater details for pharmacists undertaking the programme on what is expected of them in practice to reach the required standard.
Domains, capabilities, outcomes and descriptors
DOWNLOAD PDF DOCUMENT
Core clinical assessment skills
The core set of clinical assessment skills in which post-registration foundation pharmacists must be competent to perform by the end of their programme are:
- Blood pressure (manual and automated)
- Heart rate and rhythm (manual and automated)
- Temperature
- Respiratory rate
- Peak expiratory flow rate
- Peripheral oxygen saturation
- Urinalysis
- Height, weight, BMI
- Blood glucose (capillary)
- Capillary refill time
- Calculate NEWS 2 to identify deteriorating patients
- Mental and cognitive state examination
- Depression and anxiety screening
Post-registration foundation pharmacists must be able to outline the indications for these assessments, demonstrate the correct technique, follow the appropriate procedures for gaining valid consent, and perform the assessments in an appropriate setting taking account of confidentiality, consent, dignity and respect.
While being able to perform all of the clinical assessment skills competently and independently in practice is desirable, it is recognised that some work settings may not have the services or equipment to be able to provide training within the workplace and alternative learning opportunities will be required e.g. simulated training in a clinical skills lab or supported to undertake learning in another work setting.
The clinical assessments skills required by pharmacists are likely to evolve as new services are commissioned and the list will be updated accordingly.
Entrustable professional activities
Entrustable professional activities (EPAs) are units of professional practice (activity, task, area of work) which can be entrusted to learners once they have attained sufficient competence. Performing the activity independently, without direct supervision is regarded as the threshold for independent practice.
The EPAs included in this curriculum prioritise activities within the prescribing process and have been selected to:
- Provide a more holistic evaluation of the learner’s ability to undertake prescribing activities
- Represent high risk activities that must be undertaken safely and effectively
- Ensure person-centred care and shared decision making throughout the prescribing process
The EPAs should be assessed within the learner’s scope of practice which has been agreed with their line manager as part of the requirements for undertaking their formal prescribing training.
This will determine the presentations and conditions which would be suitable to clinically manage during an EPA assessment. The clinical encounters should be of sufficient complexity to require application of clinical reasoning, professional judgement, prioritisation and clinical decision making skills.
In all cases, the learner should demonstrate a systematic and structured approach and work within their own limitations, seeking help or referring to others as appropriate.
When the pharmacist has achieved the prescribing outcomes (see assessment blueprint) and been signed off for the clinical assessment skills, they can arrange with their DMP/DPP or an appropriate Practice Supervisor to undertake the EPA assessment.
Each EPA requires the learner to be able to demonstrate several outcomes across different domains. Depending on the clinical encounter, more than one EPA may be covered during the individual assessment encounter.
The EPA will be attained when the learner:
- can demonstrate the knowledge, skills and behaviours required of the activity
- knows when to ask for additional help and is trusted to do so in a timely manner
The learner is then entrusted to undertake the activity with reactive supervision i.e. on request and quickly available.
The EPAs support the DMP/DPP decision making process that the learner’s prescribing practice is safe and prioritises patient safety. EPAs are a curriculum requirement for all learners undertaking an integrated training programme and are optional for those undertaking a modular training programme where independent prescribing is delivered through a standalone HEI course.
The EPAs included in the programme of learning are (see below and the full curriculum document for more detail):
EPA 1: Clinical assess individuals, incorporating the consultation, examination, and relevant investigations
The pharmacist communicates effectively and establishes a partnership with the person and their carer/family. They undertake a person-centred and structured consultation in an appropriate setting taking account of confidentiality, consent, dignity and respect. They use clinical reasoning to gather focused information (full medical, social and medication history) and select appropriate examinations and investigations relevant to the person and their presenting complaint. They undertake appropriate physical and non-physical assessments, understand the significance of any abnormal findings and act in an appropriate and timely manner.
The findings are recorded in a structured and logical way. Recognition of complex cases should happen early, with advice sought from more experienced colleagues or appropriate referral within an appropriate timescale.
EPA 2: Formulate differential diagnosis and initial management plan

The pharmacist integrates and interprets the information from the consultation, examination and investigations to formulate the differential diagnosis*. This should be discussed with the person and their carer/family, and through a shared decision making process (where appropriate), agree a mutually acceptable initial management plan which reflects the evidence base, manages uncertainty and clinical risk, considers the person’s ideas, concerns and expectations, and prioritises care appropriately.
The plan should include clear benefit-risk assessment and monitoring parameters, frequency and timescale as appropriate. The pharmacist considers the person’s health literacy, provides tailored information and adapts communication in a way that is responsive to the person and their carer/family’s communication and language needs, preferences and abilities. The pharmacist ensures the person and their carer/family understand the management plan including arrangements for follow up and monitoring of efficacy and side effects.
* the list of conditions a pharmacist is expected to be able to diagnose will be linked to their scope of practice and the service provision within their work setting. Where the presenting condition is complex and falls out with the competence of the pharmacist, a more experienced prescriber is required to make the diagnosis and such an encounter would not be considered suitable to support an EPA decision. At all times, the pharmacist should work within their boundaries of clinical practice.
EPA 3: Recommend prescribing interventions that are evidence based, cost-effective and tailored to the person's needs and conditions

The pharmacist explains the rationale for and discusses the treatment options with the person and their carer/family, in light of their individual circumstances, to support shared decision making. They consider individual factors that might influence prescribing decisions such as co-morbidities, physiological changes associated with age, swallow ability, and attitudes and beliefs. The pharmacist critically evaluates the evidence base and uses guidance/formularies to inform prescribing decisions. Where there is uncertainty, they apply clinical reasoning and professional judgement to make safe and logical decisions which optimise clinical risk. The pharmacist proactively recommends treatment options which take account of previous side effects/adverse drug reactions, interactions, contraindications and co-morbidities. Prescribing interventions involve adding, stopping, stepping down and / or optimising medication. The choice, dosage regimen, route of administration and formulation are appropriate for the person. The pharmacist makes recommendations to a qualified prescriber and collaborates with the multidisciplinary team to optimise the person’s care. Safe prescribing practice is promoted throughout, ensuring prescriptions are unambiguous and legal.
EPA 4: Adapt management plan in response to ongoing monitoring and review of the person's condition, treatment outcomes, and preference
The pharmacist monitors and reviews the management plan through a variety of means including but not limited to discussion with the person, reviewing laboratory results, monitoring treatment outcomes, repeating clinical assessments and checking medication adherence. If necessary, the plan is adapted following a review of the person’s response to treatment, adverse effects and preferences. If required, the pharmacist takes appropriate steps to adjust medication and any adverse events are identified and managed appropriately, including reporting via the Yellow Card scheme and local reporting mechanisms. Any changes are discussed with the person and their carer/family and other members of the healthcare team and documented as appropriate.