3. Supporting pharmacists to improve outcomes for people with Type 2 diabetes
3.1. Pharmacists should work in collaboration with other healthcare professionals to play a greater role in prevention and detection services for type 2 Diabetes.
All pharmacy organisations should promote the role of pharmacists to help tackle type 2 diabetes.
Prevention
438 million people visit a community pharmacy in England every year. Pharmacies are accessible settings at the heart of communities, a perfect place to provide preventative services. 81% are already Healthy Living Pharmacies (HLPs), providing a range of prevention and detection services via a structured framework. Many provide advice on healthy eating, weight loss, stop smoking services and physical activity, thereby supporting people to self-care.
The NHS Diabetes Prevention Programme (NHS DPP)16, a collaboration between NHS England, Public Health England and Diabetes UK, was launched in 2016 to help deliver at scale evidence-based behavioural interventions for individuals identified at being at high risks of type 2 diabetes. To date, this programme has seen over 250,000 people referred into it with early positive outcomes. Pharmacists are uniquely placed to be included and help support the implementation of DPP, working with DPP providers to increase capacity and improve access for the programme.
Pharmacists across the breadth of primary care can provide support services outside of their ‘traditional’ clinical or healthcare settings to their local communities such as health and wellbeing messages, education, training and point of contact testing. Some pharmacies currently provide support to schools, community centres, supermarkets, places of worship, charity and community groups. Across England such approaches would help raise the awareness of type 2 diabetes and how best to prevent the condition from developing.
In addition, the pharmacist workforce has a wealth of diversity and represents people from many cultural, religious and socioeconomic backgrounds. The accessibility of pharmacists in the community alongside their knowledge and skills can help break down language and cultural barriers associated with the prevention and management of type 2 diabetes. This is especially important in areas of high deprivation and rural areas.
EXAMPLE: LMCP Carelink in Manchester and Trafford provides a service to the South Asian population. The pharmacist played a crucial role in a workshop aimed at tackling the growing problem of diabetes in this population, as many individuals didn’t properly understand their medication. The pharmacist advised them to discuss any issues with the relevant health professionals, rather than not take their medicines
Community pharmacies are ideally placed to build on the existing Healthy Living Pharmacies (HLPs) model and support the provision of further prevention services such as NHS Health Checks as recognised in the NHS LTP.
Detection
Early detection of type 2 diabetes would have a significant impact on the NHS and substantial health benefits to the population in England. The NHS RightCare diabetes pathway demonstrated that over 5 million people in England have high blood sugar (pre-diabetes/non-diabetic hyperglycaemia) which places them at significant risk of development of type 2 diabetes. It has been predicted that over half a million people in the UK have undiagnosed type 2 diabetes, many of whom receive little or no interventions or support.
A shift towards a more clinical and quality outcome focussed community pharmacy model could help support public health screening and earlier detection of people at risk of developing type 2 diabetes. Alongside this, such opportunities would help identify people living with type 2 diabetes who are currently undiagnosed.
Screening to identify type 2 diabetes, followed by early treatment has been found to reduce cardiovascular risk factors16a. Therefore, consideration should be given to providing additional services such as validated point of contact HbA1c testing, blood pressure screening and cholesterol testing through the pharmacy.
Across primary care, pharmacists can have an active role in identifying people at high risk of developing type 2 diabetes. This can be via structured case findings. Case finding approaches across PCNs should be used to identify any people who are at high risk of, or undiagnosed with, type 2 diabetes. Many pharmacists working in general practice and across CCGs are already providing such services, but there needs to more consistency across England. Another method to support the identification of people at high risk of development type 2 diabetes should include the community pharmacy quality payment scheme.
To help develop and achieve new ways of working, service delivery and greater integration with community and primary care services, there needs to be the development of an infrastructure to enable the improvement and expansion of joined-up out of hospital care for people with type 2 diabetes.
New referral and communication systems between community pharmacists, GP practices and hospitals would improve the continuity of care of people with type 2 diabetes, preventing duplication of work, optimising workload and enabling the safe transfer of patients and relevant information across care settings. This could be explored via the new local health and care records (LHCRs).
Another method to support the identification of people at high risk of development type 2 diabetes should include the community pharmacy quality payment scheme.
Preventing people from developing type 2 diabetes is one of the most significant challenges faced by the NHS. The NHS LTP commits the NHS to population health management solutions to understand health needs and match NHS services to them. Pharmacists and their teams must to be included as part of the solution. There needs to be better pharmacist engagement with local commissioners and local authorities need to promote the role of pharmacy teams in prevention and early detection.
Make local pharmacy leaders part of the strategic planning and operational delivery of PCNs and ICSs. Pharmacists are part of the solution to improving prevention and early detection of type 2 diabetes and it is important systems consider how they will use the pharmacist workforce to support people with type 2 diabetes.
EXAMPLE: I joined the Royal Air Force at the age of 19 and left when I reached 44. During those years, aircrew medical examinations did not suggest diabetes. Nor did later Civil Aviation Authority (CAA) medical examinations, which continued until my retirement at 60.
Now at the age of 61, free diabetes testing at my local pharmacy diagnosed a blood glucose level of 6.2%. I immediately changed my diet and lifestyle, allowing me to remain free of medication for the next 12 years until I was prescribed “Metformin” 500mg twice daily.
- MS, Patient aged 74
3.2. Pharmacists should play an active role in optimising medicines, improving the health, wellbeing and safety of people with type 2 diabetes across the NHS
Pharmacists should promote better patient understanding of, and engagement with, their type 2 diabetes and ensure safer and optimal use of medicines.
The World Health Organisation (WHO) Third Global Patient Safety Challenge ‘Medication Without Harm’, aims to halve severe and avoidable medication-related harm by 202017. Up to 50% of people do not take medicines as intended18. Helping people to take their medicines would improve the health of the population more than any specific medical treatment19. According to a report from 2010 if medicines were used in an optimal manner20 up to £500 million could be generated in just five therapeutic areas including diabetes.
Generally, people with type 2 diabetes will have one or more medicines prescribed for them, with people over 65 years old with type 2 diabetes having on average 6-7 comorbidities20a. Using pharmacists’ clinical skills and expertise to work in collaboration with other healthcare teams across a system will help people with type 2 diabetes to get full benefits from their medicines. Pharmacists play a leading role in the optimisation of medicine regimens, ensuring appropriate use of medicines and stopping medicines (‘deprescribing’) where appropriate. In addition, pharmacist can lead on opportunities for non-pharmacological interventions such as lifestyle changes, low-calorie diet approaches and social care prescribing as referred to in the NHS LTP.
More advanced symptoms of diabetes, or poorly controlled diabetes, perhaps due to people not taking their medicines as intended, will lead to poor health-related outcomes and macrovascular complications associated with type 2 diabetes. Pharmacists can recognise this and make appropriate clinical interventions while being able to offer advice to patients and healthcare professionals.
It is important that people with type 2 diabetes have their medicines reviewed routinely by a pharmacist. Alongside optimising medicines, pharmacists will ensure appropriate monitoring occurs and support the completion of a person’s type 2 diabetes "15 Diabetes Healthcare Essentials", for example, eye screening or foot checks.
Adopt an individualised approach to diabetes care that is tailored to the needs and circumstances of adults with type 2 diabetes, taking into account their personal preferences, comorbidities, risks from polypharmacy, and their ability to benefit from long-term interventions because of reduced life expectancy. Such an approach is especially important in the context of multimorbidity. Reassess the person’s needs and circumstances at each review and think about whether to stop any medicines that are not effective.’
- NICE Type 2 Guidance
Pharmacists working with and in Primary Care Networks (PCNs) can support people with type 2 diabetes through:
- Patient-facing clinic-based roles
- Structured Medication Reviews
- Long-term condition clinics
- Supporting people taking multiple medicines
- Improving antimicrobial stewardship
- Supporting care homes
- Data-driven care approaches to identify people who would benefit from care planning.
- Linking with pharmacists in other sectors
EXAMPLE: AT Medics provides General Practice services spread across 16 CCGS. They did not employ any pharmacists before 2015, but now have over 30 practice-based pharmacists. A 2017 project aimed to use the in-practice pharmacists to improve performance against the eight care processes and three treatment targets of the National Diabetes Audit. There was a huge reduction in variation between the highest and lowest performing practices. 86% of patients with type 2 diabetes had received all eight care processes (an improvement of 46%) and 48% had achieved all three treatment targets (an improvement of 7%). These results were higher than any CCG in the UK during 2017/18.
As part of the Getting IT Right First Time (GIRFT) programme, pharmacists in hospitals have a key role to play in helping reduce unwarranted variations across all speciality areas including diabetes care in specialist units, looking at areas such as safety. Insulin errors are common in the hospital setting, may cause significant harm, and can significantly delay hospital discharge. Data from the NADIA audit 2017 showed that nearly 1 in 5 patients experienced an insulin error, with almost a third (31%) experiencing a diabetes medication error. Due to the common nature of diabetes medication errors, pharmacy departments within hospitals should have an ongoing strategy to reduce diabetes medication errors as part of a high-risk medicine’s safety plan.
With around 15-20% of hospital patients having diabetes and the significant proportion that experience a medication error hospital trusts should have a specialist pharmacist that works within or closely alongside the inpatient diabetes service to ensure there is shared departmental responsibility for reducing diabetes medication errors and improving diabetes safety within hospital settings.
Seamless care for people requires hospital pharmacy teams to play a leading role in providing safe and effective clinical handover and discharge to primary care and community services. Pharmacists working within PCNs play an important role in supporting medicines reconciliation at the point of discharge and work collaboratively with hospital and community pharmacy colleagues. Alongside this, the New Medicines Service (NMS) can be further utilised to support and educate people who have been started on new medication in hospitals relating to diabetes.
Data has demonstrated readmission rates are lower, and hospital stays shorter for patients who have received community pharmacist follow-up consultations21. National adoption of The Transfer of Care Around Medicines (TCAM) project has the potential to save £28.8 million in 2019-20, based on a reduction of hospital length of stay by 113,406 days and 2,007 fewer readmissions22.
Pharmacists across the healthcare system can help support people with self-management of their conditions. Significant improvements can be made post-diagnosis through greater educational support, lifestyle changes and social care prescribing interventions. Pharmacists in primary care and community services can play a leading role in identifying diabetes complications early, refer patients to appropriate healthcare professionals and identify people who may benefit from greater personalised care approaches. PCNs should explore the opportunities for pharmacists to undertake social care prescribing and ensure they are actively involved in personalised care plans.
Furthermore, people with diabetes can experience high rates of mental health problems such as depression, anxiety and eating disorders. It is important that all people with diabetes have easy access to psychological support and treatments to reduce psychological distress and improve self-management. Pharmacists should be supported to play a greater role in the psychological and emotional support of the mental health and wellbeing of people with type 2 diabetes.
For those people with severe mental illness, commissioners should set out a requirement of local diabetes services to support mental health services by training them in the key monitoring and care of people with diabetes.
- NHS RightCare
Sustainability and Transformation Partnerships (STPs), Integrated Care Systems (ICSs) and Primary Care Networks (PCNs) must include pharmacists and their teams. This can be achieved by building collaborative services between healthcare professionals supporting a local population health which focuses on medicines optimisation, personalised care, shared decision making and consistent messaging.
3.3. Pharmacists in specialist and generalist roles should be given access to the most up to date education and training to support people with multiple conditions.
The RPS will work with national NHS organisations and education providers to support post-graduate education for generalists, specialists and consultant pharmacists who care for people with diabetes, underpinned by RPS professional curricula.
Pharmacists are already involved in the care of people with diabetes at all stages; from prevention and detection, supporting them with their medicine use, and all the way through to specialist services delivered by consultant pharmacists.
Pharmacists using their consultation and coaching skills can help support behavioural change, personalised care approaches and be part of shared decision making with people, their families and carers. They play a significant role in helping people understand diabetes and what it means for their lives.
Pharmacists need access to core knowledge and skills to provide improved services across all areas of healthcare. This will increase confidence in pharmacists and their teams. The RPS will work with the NHS and education providers to develop post-graduate education to deliver generalists, specialists and consultant pharmacists caring for people with diabetes, using the RPS professional curricula.
Curriculum content should ensure that pharmacists know the pathophysiology, pharmacology and treatment of diabetes, as well as public health advice. Knowledge of cultural factors such as prevalence in different population types should also be included.
3.4. NHS organisations need to establish and embed the role of consultant pharmacists in diabetes across the NHS should ensure improved outcomes in the management of people with type 2 diabetes, promote collaborative practice, multidisciplinary team working, quality improvement and research.
The NHS needs to increase the number of advanced practice and consultant diabetes pharmacists to offer diabetes advice and support across the health system.
The pathway from foundation to advanced generalist and specialist pharmacist and on to consultant pharmacists needs to be clear (see graphic below), and more outreach models are required, so specialist pharmacists can deliver care where needed by the public. The RPS has a leading role in the development of standards, curricula and assessments to underpin post-registration training. A new Foundation Pharmacist Framework is in development and the Advanced Pharmacy Framework is well established.
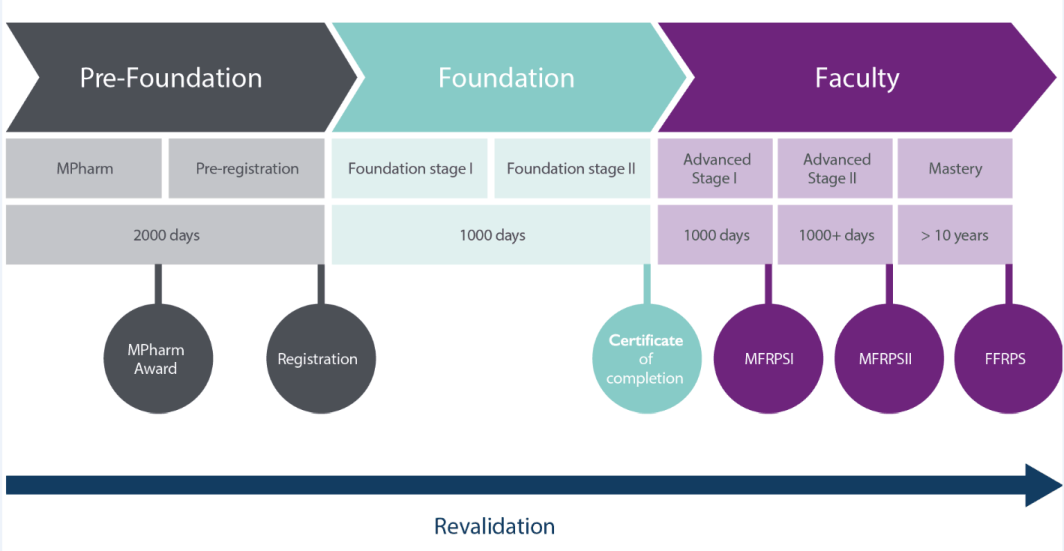
Figure 1: The RPS Pharmacist Careers Roadmap
Advanced practice diabetes hospital pharmacists have a role in developing policies and providing guidance related to diabetes.
As leaders in the field of diabetes and the profession, consultant pharmacists provide expert care to people with the most complex needs as well as providing advice to the teams caring for patients. Their influence spreads across organisational and professional boundaries to support the health of those accessing services in their area of practice as well as the wider population. They actively develop knowledge through research, innovate in their area of expertise, share these developments to improve care and lead on the adoption of NHS and professional priorities in their area of practice.
They are an expert resource with influence across the healthcare system as well as contributing to and driving the national strategy both within their area of practice and the pharmacy profession. They act as a mentor to peers as well as other members of the wider healthcare team.
In line with recently updated guidance on consultant pharmacist posts, pharmacists wishing to be appointed into these roles must be suitably credentialed as such and the post should be approved as having met national requirements25. Consultant Pharmacist credentialing is currently being developed by the RPS which will provide a clear description of the capabilities required for this role; diabetes will be a recognised specialty within this process.
There are currently only two Consultant Pharmacists in diabetes nationally since the introduction of consultant pharmacists in 2005. If we are to develop the pharmacy workforce to increase the number of specialist pharmacists in diabetes and support the education of generalist pharmacists managing diabetes, then we must also support the creation of consultant pharmacists posts as regional and national leaders. Organisations should explore the need for development of these posts working closely to ensure role and scope are optimised.
3.5 Use of data and technology
Technology advancements will enable the pharmacy workforce to help support and care for people with diabetes more effectively.
The Topol Review26 made recommendations that will enable healthcare professionals to make the most of innovative technologies such as genomics, digital medicine, artificial intelligence and robotics to improve services. The recommendations from the review supports the aims of the NHS LTP, the NHS Workforce Strategy (known as the ‘People’s Plan’), helping to ensure a sustainable NHS.
Achieving ‘enhanced’ medicines optimisation requires digital systems to capture, analyse and make use of patient-level health informatics27. Some areas where this would benefit include:
- Improved identification of people with diabetes who need to be proactively monitored and reviewed
- Digital tools to help monitor patients’ diagnosis and responses to medicines
- Reporting patient-level outcomes in relation to their medicines
- Identification of issues with adherence, concordance and harms related to patients’ medicines
- Quality improvement around cost-effective use of medicines
Having a workforce that is skilled to understand and interpret clinical data can help improve patient care and safety. To achieve this, there is a need for pharmacists to have access to training that improves their digital literacy capabilities28.
Technology is also used by people to help with their self-management of diabetes. Mobile apps are widely available and increasing being used by people to help manage their medicines and health conditions29. However, there needs to be a process to ensure these new technologies are safe, validated and accurate to use. Pharmacists can support and educate people with the use of non-invasive diagnostic technologies and digital apps to help improve care.
The NHS must continue to encourage access to and use of real-time data, interoperability and information sharing across primary care and secondary care for pharmacists (whether in community pharmacies, mental health services, care homes or GP practices). This will enable optimal seamless care, prevent avoidable medicine-related harm and improve outcomes.
16 NHS Diabetes Prevention Programme (NHS DPP)
16a The Effectiveness of Pharmacist Interventions on Cardiovascular Risk: The Multicenter Randomized Controlled RxEACH Trial, Journal of the American College of Cardiology, Volume 67, Issue 24, 21 June 2016, Pages 2846-2854
17 WHO global challenge
18 NICE Medicines Optimisation: the safe and effective use of medicines to enable the best possible outcomes
19 Adherence to long term therapies: Evidence for action. World Health Organisation 2003
20 Evaluation of the Scale, Causes and Costs of Waste Medicines, November 2010
20a Adapting clinical guidelines to take account of multimorbidity BMJ 2012;345:e6341
21 New transfer of care initiative of electronic referral from hospital to community pharmacy in England: a formative service evaluation
22 The AHSN Network – Transfer of Care Around Medicines
25 SPS – Specialist Pharmacy Services – Draft Consultant Pharmacist Guidance August 2018
26 The Topol Review – Preparing the healthcare workforce to deliver the digital future
27 The Topol review and pharmacy
28 A Health and Care Digital Capabilities Framework – HEE
29 NHS Apps Library