How the framework was updated
The review involved strategic support and engagement with wider stakeholders through a multi-disciplinary, external task and finish group from across the UK. The task and finish group concluded the 2016 framework was broadly fit for purpose, based on a literature view and extensive use of the framework in practice and confirmed a need for an update and refresh. The process used to update the framework is proportionate to that view and reflects an iterative development of the competencies.
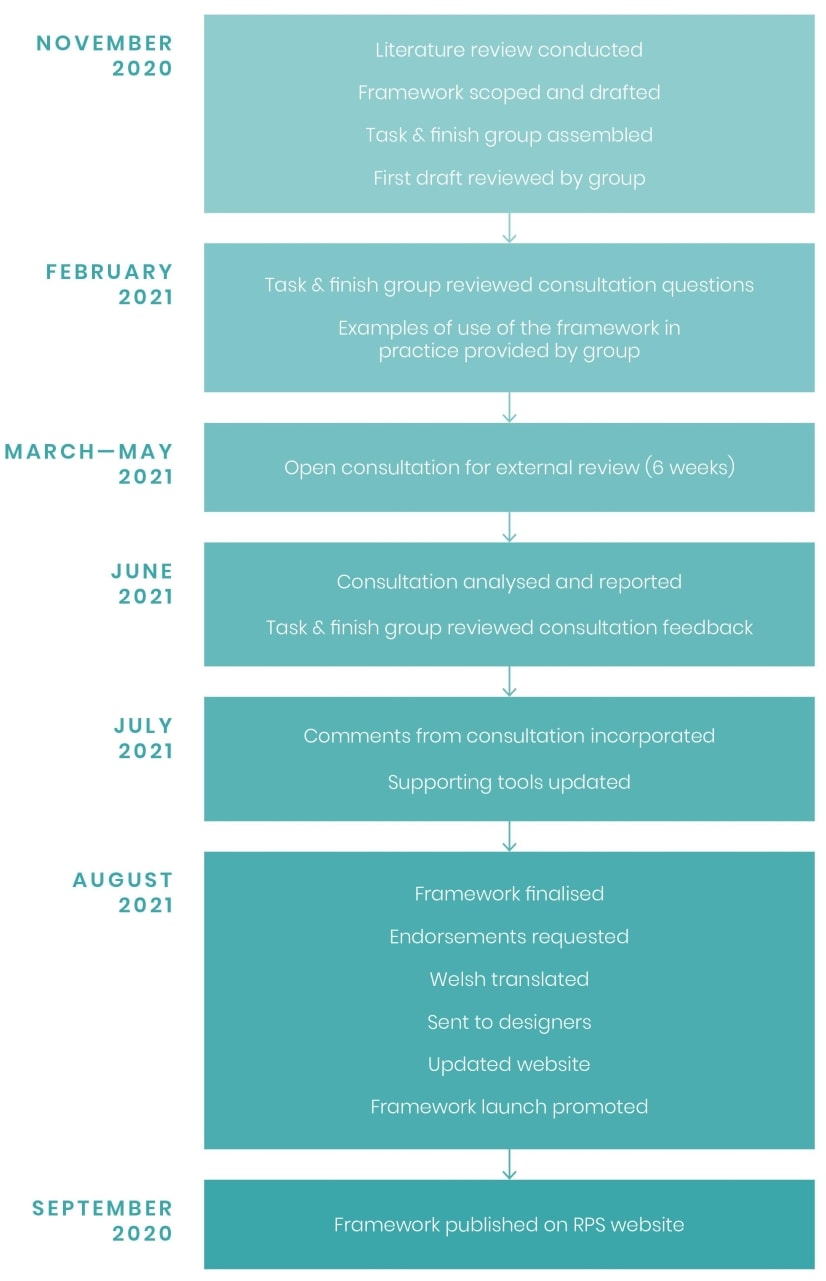
The process used to update the framework is illustrated below:
Multi-disciplinary engagement
The framework is used by a range of healthcare professions.
A multi-disciplinary external task and finish group comprising representatives from professional regulators, professional organisations, prescribers from all prescribing, lay representatives and other relevant and interested stakeholder groups from across the UK was created to review and update the framework. The group was chaired by Angela Alexander and all members of the task and finish group were asked to declare conflicts of interest which were managed in line with RPS policy.
The review consisted of three virtual discussions during the duration of 10 months aligned to key milestones (see timeline below). Meetings were held with the group to keep members of the group informed about progress and to stimulate discussion about improvements to the framework, and how the framework might be promoted and used once published.
For further information on the members of the task and finish group, please see ‘Acknowledgments’.
Development process and timeline
Literature review
A literature review was undertaken in November 2020 to identify key changes and evidence relating to competency and good practice in prescribing since the publication of the 2016 framework.
For further information please see ‘Literature review'.
Task and finish group
The task and finish group consisted of representatives from:
- British Dental Association
- Chartered Society of Physiotherapy
- College of Paramedics
- General Pharmaceutical Council
- Health and Care Professions Council
- Health Education and Improvement Wales
- National Institute for Health and Care Excellence
- NHS Education for Scotland
- Nursing and Midwifery Council
- Representatives from across all prescribing professions, academia, primary and secondary care, and lay representatives
- Royal College of General Practitioners
- Royal College of Nursing
- Royal Pharmaceutical Society
- Society and College of Radiographers
- The College of Optometrists
- The Royal College of Midwives
- We also had colleagues from across England, Scotland, Wales and Northern Ireland.
The group discussed proposed changes by RPS and provided strategic oversight in the update of the framework to ensure the competencies are still current, in scope and fit for purpose for all prescribers.
The task and finish group used a consensus process to review and update the framework in the context of the literature review.
The multidisciplinary nature of the group ensured the generic nature of the framework was maintained. The group ensured the changes were in line with current prescribing practice and were understandable to prescribers.
For further information on the updates and changes made, please see 'Summary of changes made to the framework'.
Consultation
A draft copy of the revised framework was posted on the RPS website for six weeks for open consultation from 26 March 2021 to 7 May 2021. The task and finish group were all asked to draw attention to the availability of the framework for comment.
There were 25 questions and 273 responses to the consultation received. Results were analysed and comments from the consultation were reviewed by the task and finish group. Those that were in scope and relevant were incorporated into the framework. The group used a consensus process to agree all final amendments to the framework.
Endorsement
Organisations who endorsed the 2012 version of the framework were invited to continue to endorse the framework. Other relevant organisations were also invited to endorse the framework.
For further information on who endorsed the framework, please see 'Who endorsed the framework'.
Supporting tools
In response to the consultation feedback and to support the uptake of the framework, we have produced the following:
- Examples of uses of the framework in practice
- Ways of demonstrating/evidencing competencies
- Word template of the framework
- PowerPoint presentation about the framework
- Supporting resources for the framework - useful links to further information
- Competency Framework for Designated Prescribing Practitioners
- Welsh translated version
- Updated website - improved navigation and open access.
For further information on the supporting resources and tools please see 'Supporting tools'.
Promotion
RPS will work with the pharmacy profession to encourage uptake of the framework in practice.
We will also liaise with the professional bodies and organisations of the other prescribing professions and would expect them to work with their stakeholders to encourage uptake.
Where opportunity for joint working across the professions arises we will contribute.
Statement of funding
The update to this framework has been wholly funded by the RPS who has not received any payment from a third party for its development.
For further information on how the RPS is funded, please see our Professional standards, guidance and frameworks process development manual.
Consensus statement
The task and finish group used a consensus process to agree the final version of A Competency Framework for all Prescribers. Consensus was achieved.