Case study 3
Community pharmacy Warfarin clinic
A community pharmacist based in Hywel Dda LHB, West Wales has established a Warfarin clinic where she utilises her IP status routinely to ensure patients anticoagulant therapy is managed close to home.
Previously, patients would have attended an INR Clinic at a hospital for monitoring. For one gentleman, who is a regular patient at the pharmacy, this involved driving over 30 minutes each way and spending up to 2 hours at the
hospital depending on the number of patients waiting at the clinic.
On one occasion, three attempts were made to draw blood via a venous sample. Even after these attempts, there was insufficient blood for the laboratory to test and the patient had to travel back to the hospital again.
The patient had found the episode extremely upsetting.
The patient was offered the pharmacy based INR service. Testing is done via a finger prick test and the result is immediate. During the 7 months that he has been attending the pharmacy for testing, the frequency of his INR monitoring has reduced from weekly to every 8 weeks.
This service has made a dramatic difference to patients and ensures that they have continuity of care from their already trusted community pharmacist.
- Rachel Davies, Burry Port Pharmacy Ltd
Case study 4
Pharmacist led cardiology clinics
SIGN Guideline 148 and NICE CG172 recommend treatment with Angiotensin Converting Enzyme Inhibitors (ACEI) in patients with post-myocardial infarction (Post-MI) left ventricular systolic dysfunction (LVSD)
Figure 1 below shows an example of the improvement in the use and target dosing following the introduction of pharmacist-led clinics within cardiology in NHS Greater Glasgow & Clyde.
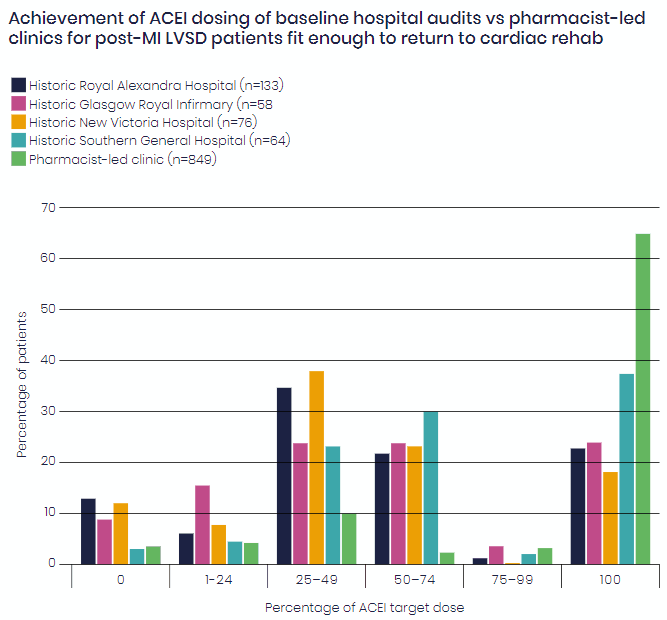
Achievement of ACEI dosing of baseline hospital audits vs pharmacist-led clinics for post-MI LVSD patients fit enough to return to cardiac rehab
See
below link- here is the formal publication for updated results:
https://bmjopenquality.bmj.com/content/8/3/e000676
- Courtesy of Paul Forsyth MRPharmS, Lead Pharmacist, Clinical Cardiology, (Primary Care) / Heart Failure Specialist