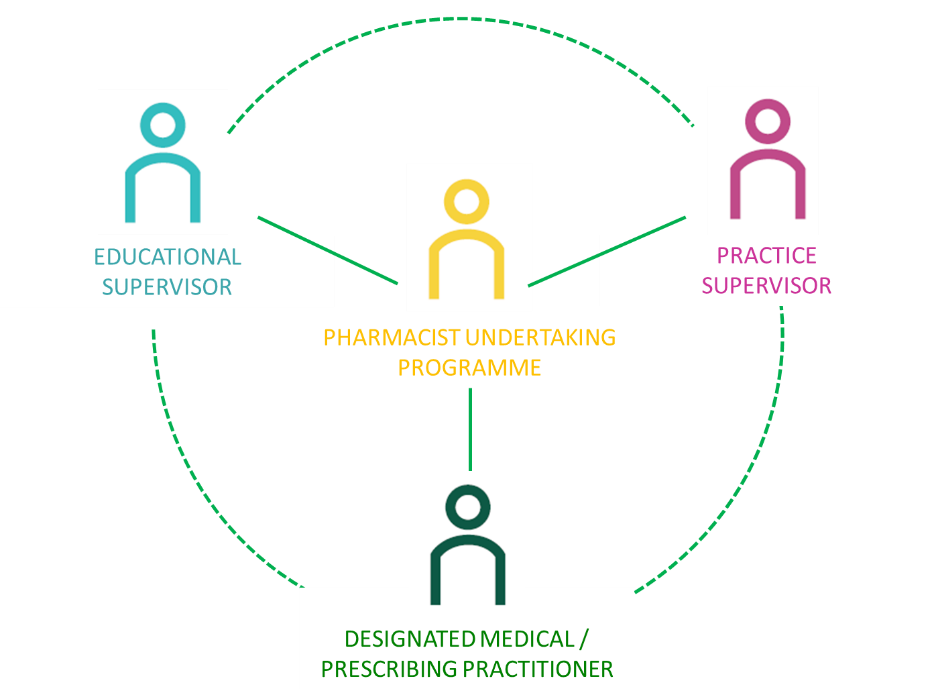
There are three different types of support roles to help you achieve the outcomes:
- Educational supervisor
- Designated prescribing practitioner
- Practice supervisor
You must have a named designated prescribing practitioner to meet the GPhC independent prescribing standards and you should also receive support from a named educational supervisor and practice supervisors. We strongly recommend you have access to an educational supervisor to guide your personal and professional development and support you to achieve the curriculum requirements.
While the roles of the different supervisors vary and are described below, it is possible that in some work settings / smaller organisations that one person may take on two or even three of these roles.
We recommend you have regular monthly scheduled and documented meetings with your educational supervisor and / or designated prescribing practitioner.
All supervisors should:
- be appropriately trained for their roles and understand the programme of learning, the educational approach and the assessment processes of the post-registration foundation programme
- be positive role models
- demonstrate cultural awareness and take active steps to promote equality and diversity, address any issues which may lead to differential attainment, and promote an inclusive culture and learning environment for all
- provide high quality, supportive and constructive feedback which is essential for the professional development of the pharmacist, and when combined with self-reflection, promotes deeper learning
Responsibility for the quality management of supervision, including training, is the role of the statutory education bodies, training provider and/or employers and should be formally agreed by partners when developing post-registration foundation programmes and associated governance structures.
Educational Supervisors

Pharmacists undertaking a post-registration foundation programme should have a named pharmacist who is responsible for the overall supervision and management of their educational progress during the programme (excluding independent prescribing). This role can be delivered remotely. The educational supervisor will help guide the pharmacist with their personal and professional development and, in addition to the skills of the practice supervisor, they should also have an understanding of educational theory. They are expected to undertake supervised learning events, monitor the quality of any evidence of learning submitted by the post-registration foundation pharmacist, provide timely and effective feedback on their progress, and guide reflective practice. In summary, the educational supervisor has overall responsibility for confirming the pharmacist has met the non-independent prescribing outcomes of the programme.
The educational supervisor should:
- understand the range of learning, assessment and support opportunities for learning in the workplace to cover the curriculum
- ensure that the pharmacist is receiving appropriate support, training and teaching
- work collaboratively with colleagues to monitor and support the pharmacist’s progression
- foster the pharmacist’s autonomy
- have a good understanding of any supporting IT tools e.g. e-portfolio and of what is considered acceptable progress
- review learning and provide formative feedback for reflective practice
- assess formal work-place evidence against the curriculum
- meet regularly with the pharmacist to review progress through the curriculum
- identify and support pharmacists experiencing difficulties, including liaising with relevant supervisor(s), interfacing with employment performance management procedures and ensuring agreed steps/actions are shared as appropriate
Designated prescribing practitioners
Pharmacists must have a named designated prescribing practitioner during the formal period of learning in practice.
Designated prescribing practitioners must meet the regulatory requirements in the GPhC Standards for the education and training of pharmacist independent prescribers, and should be able to demonstrate the competencies in the RPS Competency Framework for Designated Prescribing Practitioners. They should have the capacity to adequately undertake the role and provide the required level of support and supervision to protect patient safety. They have overall responsibility for confirming the pharmacist has met the independent prescribing outcomes of the programme and is competent to practise as a prescriber.
The designated prescribing practitioner will help guide the pharmacist with the professional development of their prescribing capabilities. They are expected to assess patient-facing clinical and diagnostic skills, monitor the quality of any evidence of learning submitted by the pharmacist, provide timely and effective feedback on their progress, and guide reflective practice. They have overall responsibility for confirming the pharmacist has met the independent prescribing outcomes of the programme and is competent to practise as a prescriber.
The designated prescribing practitioner is required to supervise the pharmacist during the period of learning in practice and during this time should:
- provide sufficient supervision and support to the pharmacist and help them to plan their period of learning in practice, identifying and facilitating relevant learning opportunities
- provide dedicated time and opportunities to work alongside the pharmacist in the clinical setting
- understand how best to teach application of clinical knowledge or a clinical skill, and adapt according to the learning style of the pharmacist
- use a variety of effective teaching methods delivered in a work-place setting
- review learning and provide formative feedback for reflective practice, encourage critical thinking, and support the pharmacist develop their prescribing skills and knowledge to be a safe prescriber
- assess formal work-place evidence against the curriculum
- meet regularly with the pharmacist to review progress with their prescribing training
- ensure that the pharmacist is working under direct supervision of an appropriately qualified healthcare professional and performs prescribing-related tasks they are competent or learning under supervision to be competent, so that patient safety is not compromised
- inform the university and educational supervisor if there are any issues or concerns relating to the pharmacist’s performance and ability to become an independent prescriber
- work in partnership with the pharmacist, other practitioners and the programme provider to confirm the competence of the pharmacist
- identify learners who are struggling, instigate initial steps in supporting pharmacists with difficulties, and ensure the educational supervisor and training provider is aware of agreed steps / actions where appropriate
Practice Supervisors
Practice supervisors are responsible for day-to-day supervision in the workplace setting. This doesn’t mean they need to physically work alongside the individual, but they should be available to support the learners and provide feedback to them on a frequent basis. Practice supervisors will integrate workplace learning with service provision by enabling the pharmacist to take responsibility for real-life patient management whilst managing risk to patient safety through effective clinical governance. They provide a safe and confidential environment for pharmacists to reflect on and discuss their work. Practice supervisors should be positive role models and should themselves have appropriate experience to effectively supervise the post-registration foundation pharmacist. To effectively deliver the curriculum, practice supervisors should be available to the pharmacist, provide teaching, learning and development opportunities based on the needs of the individual, provide regular and effective feedback, undertake supervised learning events, and be present to support the pharmacist when issues arise. Some elements of practice supervision may be delegated to suitably experienced members of the multidisciplinary team and practice supervision may be delivered remotely.
A practice supervisor should:
- understand how different Post-registration Foundation pharmacists learn best, the relevance of this to teaching and training, and is able to adapt their own style accordingly
- understand how best to teach application of knowledge or a skill, and adapt according to the learning style of the Post-registration Foundation pharmacist
- support a personalised and proactive approach to learning through learning needs analysis
- use a variety of effective teaching methods delivered in a work-place setting
- understand the importance of reflecting on and evaluating their own teaching/training
- tailor and provide effective feedback to individual Post-registration Foundation pharmacists
- use reflective discussion to support the learner to explore and manage challenges, complexity and other pressures in their roles
- identify learners who are struggling, instigate initial steps in supporting trainees with difficulties, and ensure the educational supervisor and /or designated prescribing practitioner is aware of agreed steps / actions where appropriate
All supervisors should be appropriately trained for their roles and understand the programme of learning, the educational approach and the assessment processes of the Post-registration Foundation programme. They should demonstrate cultural awareness and take active steps to address any issues which may lead to differential attainment, promoting an inclusive culture and learning environment for all. Access to high quality, supportive and constructive feedback is essential for the professional development of the pharmacist, and when combined with self-reflection, promotes deeper learning.
Responsibility for the quality management of supervision, including training, is the role of the statutory education bodies, training provider and/or employers and should be formally agreed by partners when developing Post-registration Foundation programmes and associated governance structures.